Will Medicaid Pay for Assisted Living? Your Essential Guide to Coverage
Will Medicaid pay for assisted living? The short answer is: it depends. Medicaid can cover some costs associated with assisted living, but coverage varies by state and individual needs. Understanding these nuances can help you navigate the complex process of securing financial assistance for assisted living.
Key Takeaways
- Medicaid can cover assisted living services, but eligibility and benefits vary widely by state and individual circumstances.
- Assisted living costs not covered by Medicaid may include room and board, additional medical expenses, and other care assessments.
- Exploring alternative funding options such as long-term care insurance, veterans benefits, and personal savings is essential for comprehensive financial planning for assisted living.
Understanding Medicaid and Assisted Living
Medicaid acts as a lifeline for many low-income individuals, covering various health care costs. Medicaid’s role is even more critical when it comes to assisted living. Assisted living facilities offer a home-like environment where seniors can receive help with daily activities, medication management, and more. Unlike nursing homes, which provide 24/7 medical care, assisted living communities focus on maintaining independence while offering necessary support.
Approximately 800,000 older adults in the U.S. utilize assisted living facilities, which provide less intensive care than nursing homes. Medicaid’s role in covering assisted living costs is influenced by state-specific rules and individual circumstances. Financial assistance through Medicaid can significantly alleviate the burden of assisted living expenses for seniors and their families.
What is Medicaid?
Medicaid is a federal health insurance program designed to assist low-income individuals with limited resources. It provides vital support for various medical-related care expenses, making health care accessible to those who might otherwise be unable to afford it. Does Medicaid pay for all medical expenses?
Each state administers its Medicaid program, leading to variations in coverage and eligibility criteria.
Difference Between Medicaid and Medicare
Medicaid and Medicare are distinct programs catering to different populations. While Medicaid provides coverage for low-income individuals, Medicare is primarily for those aged 65 and older, as well as certain younger individuals with disabilities.
Importantly, Medicare does not cover assisted living costs, focusing instead on eligible medical expenses and short-term care.
Medicaid Coverage for Assisted Living

Medicaid can cover various services in assisted living facilities, but the specifics depend on the state and the individual’s level of care needed. Nearly one in six assisted living residents relies on Medicaid cover assisted living for daily care services. These services can include personal care assistance, medication management, case management, and care coordination. States may also offer Medicaid waivers to help cover the costs associated with assisted living services.
The amount Medicaid pays for assisted living can vary by individual and may involve income-based copayments. States may impose additional charges. These can include copayments, coinsurance, and deductibles for nonemergency services. Grasping these nuances helps in planning and managing assisted living expenses effectively, especially when considering how much medicaid pay can impact overall costs.
Home and Community-Based Services (HCBS) Waivers
HCBS waivers are designed to provide home and community-based services to low-income individuals who require substantial care, such as seniors and people with disabilities. These waivers aim to delay the transition to nursing homes by offering essential support services within the community.
Services covered under HCBS waivers can vary significantly by state and may include transportation, housekeeping, and specialized care for memory-related issues.
Personal Care Assistance
Medicaid may cover personal care assistance, which includes help with daily living activities such as dressing, bathing, and taking medication. This support is vital for many seniors, enabling them to maintain a level of independence while receiving the necessary care in an assisted living community.
Homemaker Services
Homemaker services under Medicaid services provide essential support for daily living activities. These services can include laundry assistance, light housekeeping, and meal preparation.
Such services are crucial for maintaining a clean and comfortable living environment in assisted living facilities.
Room and Board Expenses
While Medicaid covers many aspects of assisted living, it does not cover room and board expenses. Seniors and their families must plan for these costs as they can significantly impact the overall expense of assisted living.
Alternative funding options are available to help cover these long-term care costs.
Additional Medical Costs
Assisted living facilities may have additional medical costs that are not covered by Medicaid, such as medical assessments and preventive care exams. These costs are generally not included in the monthly care fee, so it’s essential to budget for them separately.
State-by-State Variations in Medicaid Coverage

Medicaid coverage for assisted living varies significantly across different states due to the individual administration of the program. Some states provide extensive support for assisted living services, while others offer more limited assistance. As of 2024, 46 states and Washington D.C. offer some form of financial aid for assisted living through Medicaid.
Income limits for Medicaid eligibility can also vary depending on whether an applicant is applying for the State Plan or a Medicaid waiver HCBS Waiver. This variability makes it crucial for individuals to research their specific state’s policies and eligibility requirements.
Finding Your State’s Medicaid Programs
The Medicaid.gov website provides a comprehensive list of Medicaid programs by state, offering valuable information on what each state offers. Contacting local Area Agencies on Aging or your state’s Medicaid assistance office will help you understand the specific eligibility requirements for Medicaid-covered assisted living in your area.
Eligibility Criteria for Medicaid-Covered Assisted Living
Eligibility for Medicaid-covered assisted living requires both financial and functional criteria. Seniors must demonstrate low financial resources, which may involve providing documentation of income and assets. Functional needs are also assessed, requiring proof that the individual needs assistance with Activities of Daily Living (ADLs).
Applicants must reside in the state where they are applying for Medicaid and in a facility that accepts Medicaid. Taking a Medicaid Pre-Screen Test can help individuals assess their potential eligibility for benefits.
Financial Needs Assessment
To qualify for Medicaid benefits, seniors must meet specific income and asset limits. For a single senior, the income limit is $2,382 per month, while for a married couple, it can be up to $4,245. Applicants must provide recent financial statements and documentation from all income sources to prove their financial situation.
Understanding these limits is crucial for effectively navigating the Medicaid application process.
Functional Needs Assessment
To qualify for Medicaid, individuals often need to show a requirement for assistance with daily living activities. This includes needing help with at least two Activities of Daily Living (ADLs), such as bathing, dressing, or eating.
Additional medical assessments may also be required to confirm the need for these services.

Applying for Medicaid for Assisted Living
The process of applying for Medicaid for assisted living can be complex, but understanding the steps can make it more manageable. You can apply for Medicaid any time of the year. To apply, reach out to your state Medicaid agency or the Health Insurance Marketplace. An elder law attorney can provide valuable assistance in navigating the eligibility and application process.
Most states require annual recertification for Medicaid benefits. If your application is denied, you have the option to appeal or reapply. This ensures that you have multiple opportunities to secure the necessary support.
Preparing Your Application
To apply for Medicaid, you will need to gather identity and income verification documents. Some programs may also require a physician’s statement to confirm the need for personal care services.
Contacting your state’s Medicaid assistance office or visiting the Medicaid.gov website can provide additional guidance on the application process. Local agencies and elder law attorneys can also offer crucial support and advice.
Finding Assisted Living Facilities That Accept Medicaid
Finding assisted living facilities that accept Medicaid can be challenging, as no facilities are required to do so, and only about half are certified to accept Medicaid. Many facilities may not actively track or publish their acceptance of Medicaid, making it essential to inquire directly.
Some facilities may also have limited space available for Medicaid-funded residents.
Researching Facilities
To locate facilities that accept Medicaid, it’s recommended to compile a list of residences using direct Google searches rather than relying on placement agencies. Contacting the sales or marketing departments of assisted living facilities directly allows for specific inquiries about Medicaid availability.
Utilizing online directories can also help narrow down your options.
Consulting Local Agencies
Consulting local agencies can provide vital assistance in navigating Medicaid coverage for assisted living. Local resources such as Area Agencies on Aging and Medicaid Service Providers offer information and support related to assisted living.
Additionally, seeking guidance from an elder law attorney can help clarify legal and financial considerations.
Alternative Ways to Pay for Assisted Living
While Medicaid is a valuable resource, it’s essential to consider alternative payment methods for assisted living. Long-term care insurance, private funds, and veterans benefits are some options that can help cover the costs. Exploring these alternatives ensures comprehensive financial planning for assisted living expenses.
Veterans Benefits
Veterans benefits provide financial assistance for eligible individuals, offering monthly payments to help cover assisted living costs. Veterans with spouses can receive up to $2,200 a month through the Aid & Attendance benefit, while veterans without dependents can receive $1,900 a month.
Despite this, less than 5% of eligible veterans currently use the Aid & Attendance benefit.
Long-Term Care Insurance
Long-term care insurance can be a valuable resource to help cover assisted living costs, reducing the financial burden on families. Experts recommend investing in long-term care insurance before the age of 55 to ensure adequate coverage.
Additionally, premiums for this insurance may be tax-deductible, offering further financial benefits.
Using Private Funds
Personal savings, Social Security benefits, and pensions are common private funds used to pay for assisted living. Many individuals consider private funds as a viable option, providing financial flexibility for covering assisted living expenses. Understanding how to effectively use these resources can significantly alleviate the financial burden.
Summary
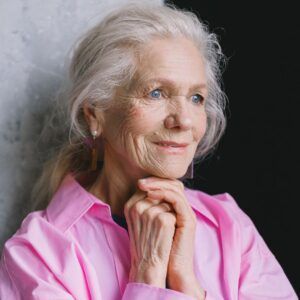
Navigating Medicaid coverage for assisted living is a complex but crucial part of planning for senior care. Understanding the differences between Medicaid and Medicare, the specific services covered, and the state-by-state variations can help families make informed decisions. Exploring alternative payment options such as veterans benefits, long-term care insurance, and private funds ensures comprehensive financial planning. At Cedar Hill Continuing Care Community, we are committed to providing guidance and support through every step of the journey, ensuring that seniors receive the quality care they deserve.
Frequently Asked Questions
Does Medicaid cover assisted living costs?
Medicaid can cover certain assisted living costs, but coverage varies by state and individual circumstances. It's essential to check your state's specific guidelines for accurate information.
What is the difference between Medicaid and Medicare?
The key difference between Medicaid and Medicare is that Medicaid serves low-income individuals, whereas Medicare is primarily for those aged 65 and older and certain younger individuals with disabilities. Additionally, Medicare does not cover assisted living costs.
What are HCBS waivers?
HCBS waivers are programs that provide home and community-based services to low-income individuals needing substantial care, helping them remain in their homes and avoid nursing home placement. This support is crucial for enhancing quality of life and independence.
How can I find assisted living facilities that accept Medicaid?
You can effectively find assisted living facilities that accept Medicaid by conducting online searches, directly contacting facility representatives, and utilizing online directories dedicated to assisted living options. This approach will ensure you gather comprehensive and accurate information.
What alternative ways are there to pay for assisted living?
You can explore alternative payment options for assisted living such as veterans benefits, long-term care insurance, and utilizing personal savings, Social Security benefits, or pensions. These methods can help alleviate the financial burden of care.